Natural Ways to Beat Diarrhoea: Achieve Regularity without the Rush
Living with Irritable Bowel Syndrome with Diarrhoea (IBS-D) can be challenging, but there are natural ways to manage and reduce the likelihood of diarrhoea.
This blog is all about pressing pause with gentle ways to ease the rush. We'll explore eight dietary and lifestyle changes that can help regulate your digestive system and make your bowel movements more predictable.
If constipation is more of a concern for you , rest assured we are working on a similar blog for you too.
1. Increase Your Intake of Soluble Fibre
Soluble fibre is a type of fibre that dissolves in water and forms a gel-like substance in the gut, which can help bulk up the stool and slow down its passage through the intestines. In contrast you may benefit from reducing intake of insoluble fibre (roughage), which can speed up gut transit and make things worse.
Good sources of soluble fibre include oats, apples, carrots and psyllium husk and partially hydrolysed guar gum. Incorporating these foods into your diet can help reduce diarrhoea and promote regularity. Try our Daily Gut Health Boosts or Hot Chocolates with 5g of PHGG in every serve.
2. Cut Down on Caffeine
Caffeine is a stimulant that can increase bowel movements and exacerbate diarrhoea. Reducing your intake of caffeinated beverages like coffee, tea and energy drinks can help manage your symptoms. Instead, opt for herbal teas or decaffeinated options to satisfy your cravings without the rush.
3. Eat on a Regular Schedule
Eating at consistent times each day can help regulate your digestive system. Try to have meals and snacks at the same time every day and avoid skipping meals. This can help train your gut to expect food at regular intervals, reducing the likelihood of diarrhoea.
4. Avoid Artificial Sweeteners
Artificial sweeteners like sorbitol, mannitol, xylitol, and erythritol can cause digestive issues including diarrhoea in some people. Check food labels and avoid products containing these sweeteners. Instead, use natural sweeteners like raw cane sugar and maple syrup in moderation.
5. Try a Low Lactose Diet
Lactose intolerance can contribute to diarrhoea and other digestive symptoms. If you suspect you may be lactose intolerant, try eliminating dairy products from your diet for a few weeks to see if your symptoms improve. There are many lactose-free alternatives available, such as almond milk (1 cup is also low fodmap), soy milk from soy protein (1 cup is also low fodmap), and lactose-free milk and yoghurt.
Our whey protein isolate-based shakes are all low in lactose (less than 2%), which most people with lactose intolerance can tolerate, but we also have plant-based options that are completely dairy free.
Out and about, you can use lactase enzyme tablets such as the Gest Dairy Primer we gave away recently. Take a tablet 20 minutes before having dairy to break down the lactase, so you don’t miss out on your favourite dishes.
6. Sip Water Steadily
Drinking large amounts of water at once can overwhelm your digestive system and lead to diarrhoea. Instead, sip water continuously throughout the day to stay hydrated without overloading your gut. Aim for small, frequent sips rather than big gulps.
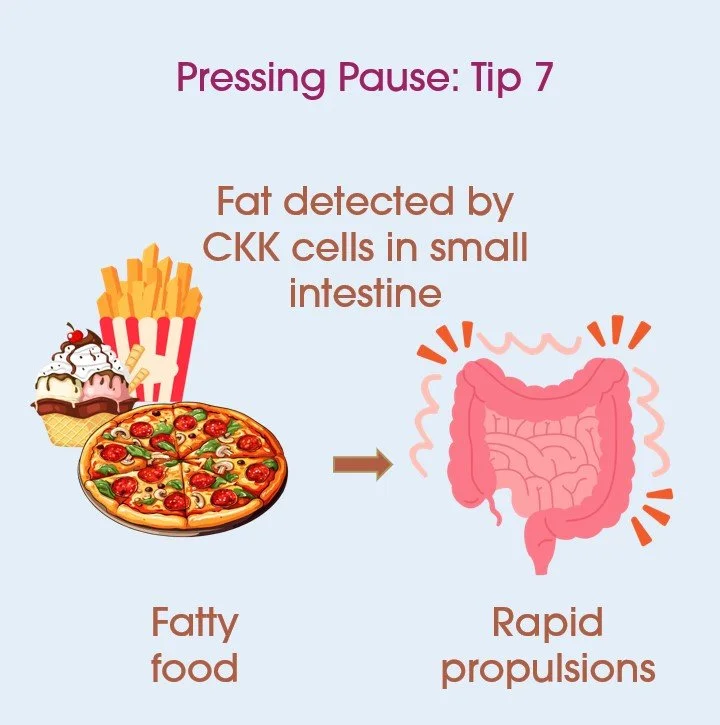
7. Limit Fatty Foods
Excessive fat intake can trigger rapid gut motility. When fat enters the small intestine, it is detected by specialised cells known as cholecystokinin (CCK) cells. These cells release the hormone cholecystokinin, which stimulates digestive enzyme secretion and gallbladder contraction to aid fat digestion. However, in individuals with IBS-D, this process can lead to excessive intestinal contractions, accelerating the movement of food through the digestive tract and resulting in loose stools and urgency. Reducing your intake of fatty foods (deep-fried food, pizza and cream), may help promote more stable digestion.
8. Consider the Low FODMAP Diet
The low FODMAP diet is a dietary approach that involves reducing the intake of certain fermentable carbohydrates that can trigger digestive symptoms in people with IBS. In particular, poorly absorbed, osmotically active molecules, such as fructose, polyols and lactose can increase water content of the small intestine with flow on effects.
This diet can be complex, so it's best to work with a dietitian to ensure you're getting the nutrients you need while avoiding trigger foods.
Conclusion
By making these dietary and lifestyle changes, you can help you to take control of your digestive health and reduce the likelihood of IBD related diarrhoea.
If these measures aren’t enough talk to your GP about medication. A combination of approaches may be needed.
We also recommend seeing your GP to achieve an initial diagnosis of IBS-D, before trying these options. Conditions like inflammatory bowel disease (IBD), coeliac disease, microscopic colitis, bile acid malabsorption, and infections can also cause diarrhoea and require specific treatment.
Blog written by: Noisy Guts co-founder Dr Mary Webberley. Mary has a background in biology, with two degrees from the University of Cambridge and post-doctoral research experience.